Imagine your gut is a bustling metropolis at the peak of rush hour. Now, envision that all the traffic lights are stuck on green due to some mysterious reason. Chaos ensues, right? That's a bit of what happens in conditions like Small Intestinal Bacterial Overgrowth (SIBO) and Leaky Gut—two gut health predicaments that often share the stage. They can turn the orderly flow of digestion into a free-for-all, leading to discomfort and confusion for anyone caught in the jam.
You may be surprised to learn that a Leaky Gut could be at the root of your depression, anxiety, thyroid problems, skin conditions, food intolerances, autoimmune diseases, fibromyalgia, and many other chronic diseases. Healthcare providers often overlook a leaky gut as a factor in chronic health problems.
Whether you're familiar with these terms or as perplexing as a foreign language menu, we will unpack the complex connection between these two gut health challenges, explore their co-occurrence, and discuss how you can naturally navigate your way to a happier, healthier gut.
SIBO - When bacteria take the wrong exit
Small Intestinal Bacterial Overgrowth, or SIBO, is like an uninvited party crasher in the small intestine. It occurs when bacteria that should be living large in the colon decide to move uptown to the small intestine, where they aren't meant to be in large numbers. These microbial misfits then feast on your meals, fermenting foods, particularly carbohydrates, causing gassiness, chronic bloating, and an array of digestive discomfort (including diarrhea, constipation, abdominal pain, nausea, etc.)
Intestinal Methanogen Overgrowth, IMO, also belongs to this category. In this case, we talk about another type of microorganism, archaea, that can also take residence in the small intestine besides bacteria. For simplicity, we will use the term SIBO in this article.
SIBO and IMO often masquerade as other digestive disorders, which makes them tricky to diagnose. (1)
Imagine taking back control of your body and living bloat-free. Download your free guide and learn the 5 MISTAKES you need to AVOID TO PREVENT SMALL INTESTINAL BACTERIAL OVERGROWTH RELAPSE.
Grab your copy today!
Leaky gut when the walls have holes
Leaky gut is a commonly used term for "Intestinal permeability," when the intestines' lining gets damaged.
Imagine your gut lining as a fortress wall, carefully guarding the sanctity of your bloodstream. This wall selectively allows nutrients to pass while keeping out harmful substances. However, when Leaky Gut rears its head, the wall is breached. Tight junctions, the security gates of your gut, become loose. Suddenly, it's less of a fortress and more of a sieve, letting particles slip into the bloodstream that have no business there—prompting inflammation and a whole host of immune responses.
In essence, Leaky Gut gives a green light to substances that should be shown the red. This not only disrupts your body's inner workings but also sets the stage for an ongoing health drama.
When intestinal cells are damaged, enzymes are also not produced for proper digestion. In this case, you may not absorb essential nutrients, leading to other diseases such as allergies, intolerances, asthma, acne, and mental disorders. There is not only a leaky gut but a leaky brain, etc. (2)
The unholy alliance - How SIBO may lead to Leaky Gut
So, how do SIBO and Leaky Gut end up in the same sentence, you ask? The connection lies in the fact that the overgrown bacteria in SIBO can produce toxins and by-products as they break down food, which can irritate and weaken the gut lining. Over time, this can turn your gut wall into something resembling Swiss cheese—full of holes and not very good at containment.
What's more, the bacteria can also consume the nutrients your cells need to maintain the gut barrier, leaving the cells weak and unable to repair themselves. This weakening is like taking bricks out of the fortress wall, one by one. Eventually, even the smallest of foes can break through.
A study (3) investigated the relationship between SIBO and Leaky Gut syndrome, and researchers found that individuals with SIBO had a significantly higher incidence of Leaky Gut syndrome.
And here's a compelling thought: just as an unhealthy gut can lead to a myriad of health issues, addressing gut health can create a ripple effect of wellness throughout the body. In this case, treating SIBO could be a key to patching up a Leaky Gut.
Testing for Leaky Gut
Diagnosing Leaky Gut requires a bit of detective work. Common signs may indicate a leaky gut, but you can also test for it.
- Intestinal Permeability Assessment: This test involves drinking a pre-measured amount of lactulose and mannitol. The levels of these sugars in the urine afterward can indicate how porous the gut lining is.
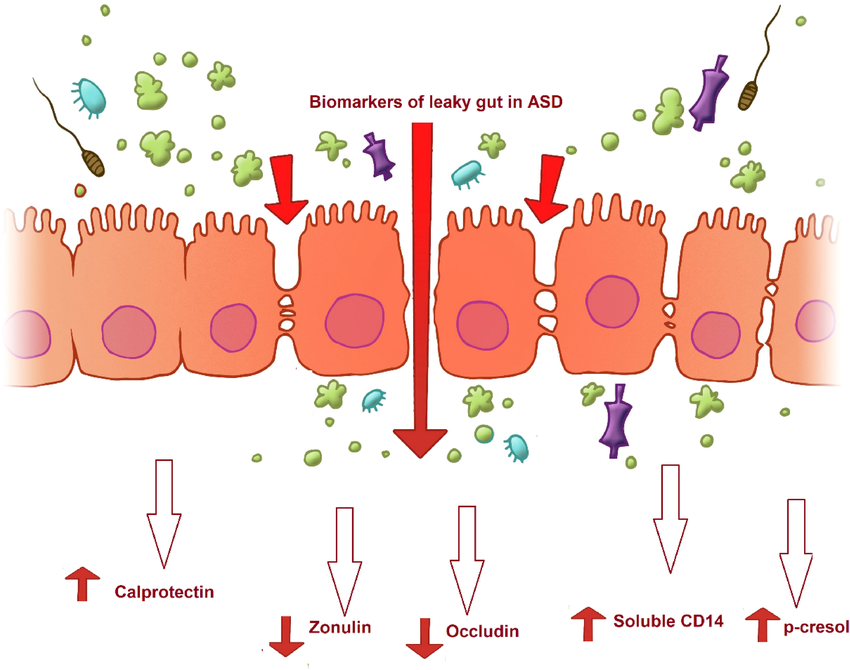
- Measuring Zonulin levels: it is a standard marker that is checked on a stool test. Zonulin controls the opening and closing of the gate, the tight junctions in your gut, allowing nutrients to be absorbed. If zonulin levels get high, the opening may take longer or be too big, and unwanted substances can leak through, causing problems. (4)
- Food sensitivity tests: These can identify which foods your immune system is reacting to, potentially as a result of particles slipping through the gut lining. Honestly, I am not a big fan of food sensitivity testing, but when somebody is reacting to many foods, it indicates that a Leaky gut may be in the background.
What causes a Leaky gut?
There are many factors outside of diet that can cause a leaky gut, such as
- SIBO (3),
- Dysbiosis (imbalance between helpful and harmful bacteria in the gastrointestinal tract),
- nutrient deficiencies (5),
- an inflammatory diet including excess alcohol, sugar consumption, gluten (6),
- chronic stress (7),
- vigorous endurance training (8),
- chronic inflammation (9),
- environmental toxins like glyphosate, mold toxicity (10), heavy metals, etc.
- infections (like Candida) (11) and endotoxins (12),
- medications (especially NSAIDs like Tylenol and Advil) (13)
Tangled connections: conditions associated with Leaky Gut
The ripple effects of Leaky Gut extend far beyond occasional discomfort; they can be associated with a variety of chronic diseases. When your intestinal barrier becomes compromised, it's like a crack in a dam, initially small and seemingly insignificant but with the potential to cause major downstream consequences. These can include:
- Autoimmune diseases: Conditions like rheumatoid arthritis, lupus, type I diabetes, and celiac disease have been linked to increased gut permeability. It's as if Leaky Gut opens the door and, in a rush, the autoimmune disorders, where the body, confused by the influx of foreign particles, begins to attack its tissues. (14)(15)
- Inflammatory Bowel Diseases (IBD): Crohn's disease and ulcerative colitis, types of IBD, may be exacerbated by Leaky Gut, as the gut's weakened defenses inflame the intestinal lining. (16)
- Irritable Bowel Syndrome (IBS): Those with IBS may find that Leaky Gut intensifies their symptoms, as their gut is already a battleground for discomfort. (17)
- Food allergies and intolerances: Like unwelcome guests slipping through a fence, food particles that breach the gut barrier can trigger allergic reactions and sensitivities. (18)
- Skin conditions: Eczema, rosacea, and psoriasis, the irritated states of our outer shell, can also be linked to what happens within our inner tube, as the gut-skin axis suggests. (19)(20)
Listening to the whispers: signs and symptoms of Leaky Gut
A leaky gut can be a silent adversary, often presenting symptoms that whisper rather than shout. Paying attention to these whispers can be key to early detection and management. Symptoms may include (21):
- Digestive issues: Chronic bloating, gas, diarrhea, or constipation
- Fatigue
- Headaches and brain fog
- Skin irritations (acne, breakouts, eczema, etc.)
- Mood swings (anxiety, depression)
- Joint pain, body pain, muscle stiffness (22)
Natural Healing for Leaky Gut
Dealing with SIBO and Leaky Gut can feel like navigating a labyrinth. However, there are natural strategies you can employ to guide you out of the maze:
Certain lifestyle and dietary changes can help you get back on track. These can include:
- Learning relaxation techniques to reduce stress levels - Never underestimate the gut-brain connection. Techniques like meditation, yoga, and Tai chi can fortify your gut against the stresses of modern life.
- Moving your body and avoiding being sedentary
- Transforming your environment by eliminating toxins (plastics, GMOs, pollutants, mold, etc.)
- Eating anti-inflammatory, whole foods and limiting refined carb intake and other food triggers
- Removing gluten (protein in wheat, rye, spelt, barley, and kamut) from the diet. Gluten has been shown to increase intestinal permeability (23)
- In case SIBO is present, a short-term low FODMAP (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) diet that aims to decrease fermentable carbohydrates may help reduce inflammation in the gut. (24)
- Getting adequate quantity and quality of sleep
- Chew, chew, chew: Digestion starts in the mouth. Chewing thoroughly is like laying a strong foundation for a building—it sets everything else up for success.
You can also support your gut lining healing with the following nutrients (22)(24):
- Bone broth or gelatin – helps the healing of the intestinal lining
- Prebiotics - feed good bacteria and boost the production of short-chain fatty acids (reintroduce them slowly and gradually if you have SIBO)
- Probiotics - help restore the gut mucous layer and prevent pathogens from overgrowth (in the case of SIBO, certain strains may work better than multistrain probiotics). Examples are L. plantarum 299v, L. rhamnosus GG, and L. acidophilus DDS-1 (24)
- L-Glutamine – an amino acid that helps repair the gut lining to regrow (25)
- Vitamins A and D - fat-soluble vitamins, have many roles, supporting the immune system (24)
- Zinc carnosine - unique support for the stomach and intestinal lining (26)
- Fish Oil – contains healthy fatty acids, such as DHA and EPA, to reduce inflammation (21)
- Curcumin (in Turmeric) - improves intestinal barrier function and reduces inflammation (27)
- Digestive enzymes - support the digestion process (24)
- Butyric Acid - serves as the primary fuel source for the colon's cells and for healing the lining of the colon and the small intestine. (28)
Of course, there are a lot of other great nutrients, herbs, and supplements that can help heal the gut lining.
Diet, supplements, lifestyle factors, and mindset all play a role in healing. You can see positive results with the right strategy within a few weeks.
Which Comes First: SIBO or Leaky Gut?
The question often arises: which condition do we address first—SIBO or Leaky Gut?
The truth is the healing order can be as unique as the individual, but a general roadmap can guide us.
The symbiotic relationship between SIBO and Leaky Gut suggests that healing one can positively influence the other. However, a common strategy among functional practitioners leans towards taming SIBO first.
Here's why:
- Quelling the bacterial tide: Addressing SIBO reduces the number of bacteria available to produce the toxins that contribute to Leaky Gut. Think of it as turning down the volume before fixing the speakers.
- Restoring balance: Once SIBO is under control, the inflammation in the gut often decreases, making it a more hospitable environment for repairing the intestinal lining.
- Avoiding a vicious cycle: If you focus solely on healing the Leaky Gut without resolving the underlying SIBO, it's like patching up a boat while still taking on water; the issue could recur or never fully resolve.
The steps to gut healing
Healing the gut is a process that requires patience and a strategic approach.
Here's a simplified order of operations:
- Eradicate SIBO: Use targeted treatments such as dietary changes, herbal antimicrobials, or prescribed antibiotics to reduce the overgrowth of bacteria in the small intestine. It is still important to uncover the possible root causes of SIBO.
- Soothe and repair the gut lining: After reducing bacterial overgrowth, support the gut with nutrients that promote healing of the intestinal lining, like L-glutamine, collagen peptides, vitamin A, etc.
- Rebalance the gut flora: Introduce or reintroduce probiotics and prebiotics to nourish and support the beneficial bacteria in your gut.
- Reinforce gut function: Implement lifestyle changes that support long-term gut health, including stress reduction techniques, regular exercise, and adequate sleep.
- Monitor and adapt: Gut healing is not linear. Regular follow-ups through testing and symptom tracking can help adjust the plan as needed.
The Importance of personalization in healing
While this sequence offers a framework, it is not a one-size-fits-all solution. The interplay between SIBO and Leaky Gut is complex, and factors such as individual health history, severity of conditions, and personal responses to treatment must shape the healing journey.
In some cases, simultaneous treatment of both conditions may be necessary, especially if symptoms are severe and quality of life is significantly impacted. For instance, a healthcare provider may recommend a gentle approach to start repairing a Leaky Gut while also treating SIBO, especially if there are strong indications of a compromised gut barrier, such as autoimmune reactions or chronic inflammation.
Closing thoughts on the healing order
Deciphering whether SIBO or Leaky Gut should be addressed first is not a universal decision. However, the prevailing thought initially steers toward gaining control over SIBO to reduce the onslaught of symptoms and create a foundation for healing the gut lining. It's a bit like calming the storm before repairing the ship.
In the voyage of gut health, understanding the healing sequence is your compass. Working with a knowledgeable healthcare provider allows you to chart a course tailored to your body's signals and needs, leading you toward smoother sailing and restoring wellness.
If you are seeking guidance in your healing journey and need personalized support, book a free Gut Strategy call, and let's discuss the first steps toward getting back control of your body and health.
This post is only for informational purposes and is not meant to diagnose, treat, or cure any disease. I recommend always consulting your healthcare practitioner before trying any treatment or dietary changes.
References:
- Bures, J., Cyrany, J., Kohoutova, D., Förstl, M., Rejchrt, S., Kvetina, J., Vorisek, V., & Kopacova, M. (2010). Small intestinal bacterial overgrowth syndrome. World journal of gastroenterology, 16(24), 2978–2990. https://doi.org/10.3748/wjg.v16.i24.2978
- Camilleri M. (2019). Leaky gut: mechanisms, measurement and clinical implications in humans. Gut, 68(8), 1516–1526. https://doi.org/10.1136/gutjnl-2019-318427
- Riordan, S. M., McIver, C. J., Thomas, D. H., Duncombe, V. M., Bolin, T. D., & Thomas, M. C. (1997). Luminal bacteria and small-intestinal permeability. Scandinavian journal of gastroenterology, 32(6), 556–563. https://doi.org/10.3109/00365529709025099
- Sturgeon, C., & Fasano, A. (2016). Zonulin, a regulator of epithelial and endothelial barrier functions, and its involvement in chronic inflammatory diseases. Tissue barriers, 4(4), e1251384. https://doi.org/10.1080/21688370.2016.1251384
- Farré, R., Fiorani, M., Abdu Rahiman, S., & Matteoli, G. (2020). Intestinal Permeability, Inflammation and the Role of Nutrients. Nutrients, 12(4), 1185. https://doi.org/10.3390/nu12041185
- Khoshbin, K., & Camilleri, M. (2020). Effects of dietary components on intestinal permeability in health and disease. American journal of physiology. Gastrointestinal and liver physiology, 319(5), G589–G608. https://doi.org/10.1152/ajpgi.00245.2020
- Konturek, P. C., Brzozowski, T., & Konturek, S. J. (2011). Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options. Journal of physiology and pharmacology : an official journal of the Polish Physiological Society, 62(6), 591–599.
- Ribeiro, F. M., Petriz, B., Marques, G., Kamilla, L. H., & Franco, O. L. (2021). Is There an Exercise-Intensity Threshold Capable of Avoiding the Leaky Gut?. Frontiers in nutrition, 8, 627289. https://doi.org/10.3389/fnut.2021.627289
- Hietbrink, F., Besselink, M. G., Renooij, W., de Smet, M. B., Draisma, A., van der Hoeven, H., & Pickkers, P. (2009). Systemic inflammation increases intestinal permeability during experimental human endotoxemia. Shock (Augusta, Ga.), 32(4), 374–378. https://doi.org/10.1097/SHK.0b013e3181a2bcd6
- Gao, Y., Meng, L., Liu, H., Wang, J., & Zheng, N. (2020). The Compromised Intestinal Barrier Induced by Mycotoxins. Toxins, 12(10), 619. https://doi.org/10.3390/toxins12100619
- Yamaguchi, N., Sugita, R., Miki, A., Takemura, N., Kawabata, J., Watanabe, J., & Sonoyama, K. (2006). Gastrointestinal Candida colonisation promotes sensitisation against food antigens by affecting the mucosal barrier in mice. Gut, 55(7), 954–960. https://doi.org/10.1136/gut.2005.084954
- Pizzorno J. (2014). Toxins From the Gut. Integrative medicine (Encinitas, Calif.), 13(6), 8–11.
- Bjarnason, I., & Takeuchi, K. (2009). Intestinal permeability in the pathogenesis of NSAID-induced enteropathy. Journal of gastroenterology, 44 Suppl 19, 23–29. https://doi.org/10.1007/s00535-008-2266-6
- Mu, Q., Kirby, J., Reilly, C. M., & Luo, X. M. (2017). Leaky Gut As a Danger Signal for Autoimmune Diseases. Frontiers in immunology, 8, 598. https://doi.org/10.3389/fimmu.2017.00598
- Sapone, A., Lammers, K.M., Casolaro, V. et al. Divergence of gut permeability and mucosal immune gene expression in two gluten-associated conditions: celiac disease and gluten sensitivity. BMC Med 9, 23 (2011). https://doi.org/10.1186/1741-7015-9-23
- Teshima, C. W., Dieleman, L. A., & Meddings, J. B. (2012). Abnormal intestinal permeability in Crohn's disease pathogenesis. Annals of the New York Academy of Sciences, 1258, 159–165. https://doi.org/10.1111/j.1749-6632.2012.06612.x
- Camilleri, M., & Gorman, H. (2007). Intestinal permeability and irritable bowel syndrome. Neurogastroenterology and motility, 19(7), 545–552. https://doi.org/10.1111/j.1365-2982.2007.00925.x
- Ventura, M. T., Polimeno, L., Amoruso, A. C., Gatti, F., Annoscia, E., Marinaro, M., Di Leo, E., Matino, M. G., Buquicchio, R., Bonini, S., Tursi, A., & Francavilla, A. (2006). Intestinal permeability in patients with adverse reactions to food. Digestive and liver disease : official journal of the Italian Society of Gastroenterology and the Italian Association for the Study of the Liver, 38(10), 732–736. https://doi.org/10.1016/j.dld.2006.06.012
- Yüksel, M., & Ülfer, G. (2022). Measurement of the serum zonulin levels in patients with acne rosacea. The Journal of dermatological treatment, 33(1), 389–392. https://doi.org/10.1080/09546634.2020.1757015
- Sinha, S., Lin, G., & Ferenczi, K. (2021). The skin microbiome and the gut-skin axis. Clinics in dermatology, 39(5), 829–839. https://doi.org/10.1016/j.clindermatol.2021.08.021
- Camilleri M. (2019). Leaky gut: mechanisms, measurement and clinical implications in humans. Gut, 68(8), 1516–1526. https://doi.org/10.1136/gutjnl-2019-318427
- Guido, G., Ausenda, G., Iascone, V., & Chisari, E. (2021). Gut permeability and osteoarthritis, towards a mechanistic understanding of the pathogenesis: a systematic review. Annals of medicine, 53(1), 2380–2390. https://doi.org/10.1080/07853890.2021.2014557
- Drago, S., El Asmar, R., Di Pierro, M., Grazia Clemente, M., Tripathi, A., Sapone, A., Thakar, M., Iacono, G., Carroccio, A., D'Agate, C., Not, T., Zampini, L., Catassi, C., & Fasano, A. (2006). Gliadin, zonulin and gut permeability: Effects on celiac and non-celiac intestinal mucosa and intestinal cell lines. Scandinavian journal of gastroenterology, 41(4), 408–419. https://doi.org/10.1080/00365520500235334
- Aleman, R. S., Moncada, M., & Aryana, K. J. (2023). Leaky Gut and the Ingredients That Help Treat It: A Review. Molecules (Basel, Switzerland), 28(2), 619. https://doi.org/10.3390/molecules28020619
- Rao, R., & Samak, G. (2012). Role of Glutamine in Protection of Intestinal Epithelial Tight Junctions. Journal of epithelial biology & pharmacology, 5(Suppl 1-M7), 47–54. https://doi.org/10.2174/1875044301205010047
- Mahmood, A., FitzGerald, A. J., Marchbank, T., Ntatsaki, E., Murray, D., Ghosh, S., & Playford, R. J. (2007). Zinc carnosine, a health food supplement that stabilises small bowel integrity and stimulates gut repair processes. Gut, 56(2), 168–175. https://doi.org/10.1136/gut.2006.099929
- Liu, X., & Zhu, H. (2022). Curcumin Improved Intestinal Epithelial Barrier Integrity by Up-Regulating ZO-1/Occludin/Claudin-1 in Septic Rats. Evidence-based complementary and alternative medicine : eCAM, 2022, 2884522. https://doi.org/10.1155/2022/2884522
- Canani, R. B., Costanzo, M. D., Leone, L., Pedata, M., Meli, R., & Calignano, A. (2011). Potential beneficial effects of butyrate in intestinal and extraintestinal diseases. World journal of gastroenterology, 17(12), 1519–1528. https://doi.org/10.3748/wjg.v17.i12.1519
- Picture: Al-Ayadhi, Laila & Zayed, Naima & Bhat, Ramesa & Moubayed, Nadine & Almuammar, May & El-Ansary, Afaf. (2021). The use of biomarkers associated with leaky gut as a diagnostic tool for early intervention in autism spectrum disorder: a systematic review. Gut Pathogens. 13. 10.1186/s13099-021-00448-y.

Alexandra is a Functional Medicine Certified Health Coach & Holistic Nutritionist specializing in IBS, SIBO, and Gut Health. She helps her clients identify the root causes of their chronic gut issues with functional testing, supporting their bodies holistically and implementing the necessary lifestyle changes long-term to regain control of their bodies and enjoy food freedom. Book your FREE SIBO Assessment call now >>>