Many people are already familiar with the term: SIBO that stands for Small Intestinal Bacterial Overgrowth. They might have been tested, treated with different approaches, and still have all sorts of digestive symptoms, or tests came back negative, then it might be the time to think of SIFO.
SIFO means Small Intestinal Fungal Overgrowth, which is a relatively new term in the medical community.
Research has found that around 25% of the people with unexplained digestive symptoms had SIFO. (1)
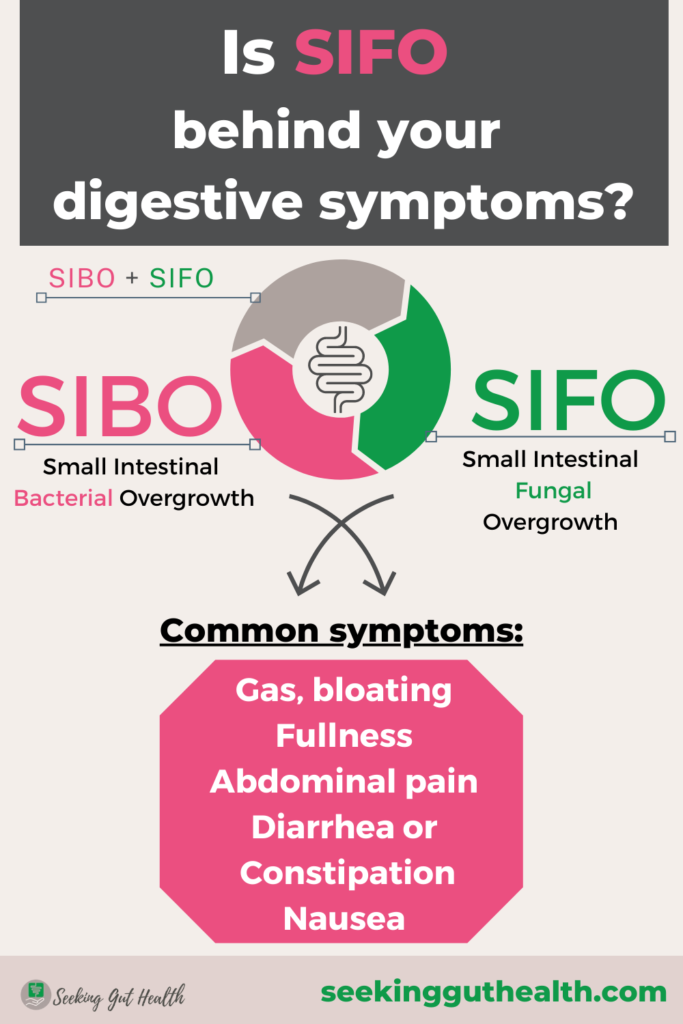
What is SIFO & what are the symptoms?
In terms of SIFO, fungi organisms colonize the small intestines causing uncomfortable gastrointestinal symptoms identical to SIBO (Small Intestinal Bacterial Overgrowth), such as:
- bloating, gas,
- belching,
- indigestion,
- abdominal pain,
- diarrhea or constipation,
- nausea,
- fatigue.
But other symptoms that may indicate the presence of fungal overgrowth emphatically could be chronic yeast infections: vaginal candidiasis, oral thrush, nail/ skin fungal infections, rashes, itching, brain fog, etc. (2)
The difference between SIBO and SIFO could be the additional symptoms present, and SIFO might not respond to the same treatment.
The research found that 97% of the fungi in SIFO come from Candida strains, such as Candida spp. or Albicans and others. (3)
How to diagnose SIFO?
While there are different testing options, like a breath test for SIBO or stool test for overgrowth of Candida, parasites, or other pathogenic bacteria in the colon, diagnosing SIFO can be difficult. The only way to diagnose is an endoscopy performed by a gastroenterologist to collect a sample of liquid from the small intestine. (4) Functional questionnaires can help assess the situation. If digestive issues remain despite previous treatment, trying an antifungal treatment might be a thing to see if it shifts the symptoms.
Imagine taking back control of your body and living bloat-free. Download your free guide and learn the 5 MISTAKES you need to AVOID TO PREVENT SMALL INTESTINAL BACTERIAL OVERGROWTH RELAPSE.
Grab your copy today!
What could be the contributing factors to SIFO?
Fungal organisms typically live in our gut with other bacteria under control without causing any symptoms. But the problem occurs when:
1. You’re immunocompromised or have a dysfunctional immune system. (5)
- Young children, older people, or people who take immunosuppressant drugs can be affected.
2. You’ve taken certain medications such as antibiotics or proton pump inhibitors (PPIs).
- PPIs are used to suppress particular cells in the stomach to inhibit acid production, reducing reflux symptoms. However, adequate stomach acid levels are required for food digestion, mineral absorption, and killing harmful organisms. Long-term usage of PPIs has been linked to SIBO and SIFO. (6)
- Antibiotics usage can negatively affect the gut microbiota causing dysbiosis – bad gut bugs or fungi can start overgrowing. They can also compromise the immune system (around 70% of the immune system can be found in the gut). (7)
3. You’ve low stomach acid levels
- Low stomach acid doesn’t just happen due to PPIs, antacids, or other acid blocker usage. Still, when you are going through a high-stress period or have chronic stress, you can get into the fight-or-flight response, and your digestive system’s function is basically shut down. Digestion is not a priority in a stressful situation.
- But it can also happen when you lack nutrients such as zinc used by your body to produce HCL (hydrochloric acid). (8) Other factors can be hypothyroidism, H. pylori infection, autoimmune conditions, cancer, age, etc.
- Signs that you lack stomach acid are excess gas, bloating, heartburn, nausea, nutrient deficiencies, burping, hair loss, etc. (9)
4. You’ve slow intestinal motility
- SIBO and SIFO can commonly occur due to dysmotility, meaning that the food is not transferred through the digestive system on time. It can be problematic because the longer the food sits in one place, particularly in the small intestine, the more bacteria or even fungi can start overgrowing where they normally shouldn’t be present.
- This can all happen due to nerve damage, surgeries, endometriosis, Ehlers-Danlos syndrome. (10)
What treatment options can help eliminate SIFO?
Try conventional or natural approaches
SIFO can be addressed with conventional antifungal drugs (like Fluconazole) or natural herbal antifungals. In many cases, practitioners combine herbal antifungals with herbal antimicrobials as a treatment option to address SIFO and SIBO simultaneously. Some of these natural agents can be olive leaf extract, oregano oil, garlic extract. (11)
Certain probiotics such as the nonpathogenic yeast, Saccharomyces boulardii, can be beneficial too. Researchers found that the probiotic S. boulardii had the same antifungal effect as Nystatin, with fewer side effects in babies. (12)
Shift your diet
Personalize your diet. Avoiding your triggering and most inflammatory foods in general, such as processed foods, refined carbs, sugar, gluten, dairy, yeast, caffeine, alcohol, and some mold-containing foods (peanuts, cashews), may help control the overgrowth. Some people choose to follow an anti-candida diet for 3-6 months. It is crucial to include many anti-inflammatory vegetables like leafy greens, healthy oils, organic meat.
Support your gut & detox pathways
Resolving a leaky gut can help calm the immune system down to fight against pathogens as well as addressing low stomach acid levels. Supporting the detoxification process is also crucial to get rid of yeast mycotoxins, especially during antifungal treatment. Opening the detox pathways could mean resolving constipation or increasing the movement of the lymph system via massage, exercise, etc.
Adjust your lifestyle
If you have poor motility, then having daily movements or even a massage can help improve your symptoms. Walking, yoga, tai chi, and other low-impact exercises are excellent.
If you tend to have slow motility, then meal spacing might be beneficial, meaning you space out your meals by 4-5 hours if possible. This way, your Migrating Motor Complex (MMC) has a chance to get activated and clear any remaining food or bacteria out of the small intestine towards the colon. If you constantly snack, then you inhibit this clearing motion. (13)
Taking care of your diet is one thing, and you may have the best diet on Earth; it is all for nothing if you eat fast without chewing your food properly or eat in a stressed state.
The Bottom Line
If you have been experiencing inexplicable digestive symptoms, it would be time to see if SIFO might play a role. The symptoms of SIBO and SIFO could be similar, but both require a holistic approach that addresses the root causes. It is vital to have a personalized protocol to ensure the best results.
*This post is only for informational purposes and is not meant to diagnose, treat or cure any disease. I recommend consulting with your healthcare practitioner always before trying any treatment or dietary changes.
Erdogan, A., & Rao, S. S. (2015). Small intestinal fungal overgrowth. Current gastroenterology reports, 17(4), 16. https://doi.org/10.1007/s11894-015-0436-2
Richardson JP, Ho J, Naglik JR. Candida-epithelial interactions. J Fungi (Basel). 2018;4(1). doi:10.3390/jof4010022
Askin Erdogan, Y. Y. (2014). Small Intestinal Fungal Overgrowth (SIFO): A Cause of Gastrointestinal Symptoms. Gastroenterology, S-358. Retrieved from https://www.researchgate.net/publication/283378174_Sa2026_Small_Intestinal_Fungal_Overgrowth_SIFO_A_Cause_of_Gastrointestinal_Symptoms
Rao SSC, Tan G, Abdulla H, Yu S, Larion S, Leelasinjaroen P. Does colectomy predispose to small intestinal bacterial (SIBO) and fungal overgrowth (SIFO)?. Clin Transl Gastroenterol. 2018;9(4):146. doi:10.1038/s41424-018-0011-x
Lamps, L. W., Lai, K. K., & Milner, D. A., Jr (2014). Fungal infections of the gastrointestinal tract in the immunocompromised host: an update. Advances in anatomic pathology, 21(4), 217–227. https://doi.org/10.1097/PAP.0000000000000016
Su, T., Lai, S., Lee, A., He, X., & Chen, S. (2018). Meta-analysis: proton pump inhibitors moderately increase the risk of small intestinal bacterial overgrowth. Journal of gastroenterology, 53(1), 27–36. https://doi.org/10.1007/s00535-017-1371-9
Francino M. P. (2016). Antibiotics and the Human Gut Microbiome: Dysbioses and Accumulation of Resistances. Frontiers in microbiology, 6, 1543. https://doi.org/10.3389/fmicb.2015.01543
Shafaghi, A., Hasanzadeh, J., Mansour-Ghanaei, F., Joukar, F., & Yaseri, M. (2016). The Effect of Zinc Supplementation on the Symptoms of Gastroesophageal Reflux Disease; a Randomized Clinical Trial. Middle East Journal of digestive diseases, 8(4), 289–296. https://doi.org/10.15171/mejdd.2016.38
Fatima R, Aziz M. Achlorhydria. [Updated 2021 Jun 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507793/
Jacobs, C., Coss Adame, E., Attaluri, A., Valestin, J., & Rao, S. S. (2013). Dysmotility and proton pump inhibitor use are independent risk factors for small intestinal bacterial and/or fungal overgrowth. Alimentary pharmacology & therapeutics, 37(11), 1103–1111. https://doi.org/10.1111/apt.12304
Samadi, F. M., Suhail, S., Sonam, M., Sharma, N., Singh, S., Gupta, S., Dobhal, A., & Pradhan, H. (2019). Antifungal efficacy of herbs. Journal of oral biology and craniofacial research, 9(1), 28–32. https://doi.org/10.1016/j.jobcr.2018.06.002
Demirel, G., Celik, I. H., Erdeve, O., Saygan, S., Dilmen, U., & Canpolat, F. E. (2013). Prophylactic Saccharomyces boulardii versus Nystatin for the prevention of fungal colonization and invasive fungal infection in premature infants. European journal of pediatrics, 172(10), 1321–1326. https://doi.org/10.1007/s00431-013-2041-4
Deloose, E., & Tack, J. (2016). Redefining the functional roles of the gastrointestinal migrating motor complex and motilin in small bacterial overgrowth and hunger signaling. American journal of physiology. Gastrointestinal and liver physiology, 310(4), G228–G233. https://doi.org/10.1152/ajpgi.00212.2015

Alexandra is a Functional Medicine Certified Health Coach & Holistic Nutritionist specializing in IBS, SIBO, and Gut Health. She helps her clients identify the root causes of their chronic gut issues with functional testing, supporting their bodies holistically and implementing the necessary lifestyle changes long-term to regain control of their bodies and enjoy food freedom. Book your FREE SIBO Assessment call now >>>